H. pylori Antibody Rapid Test
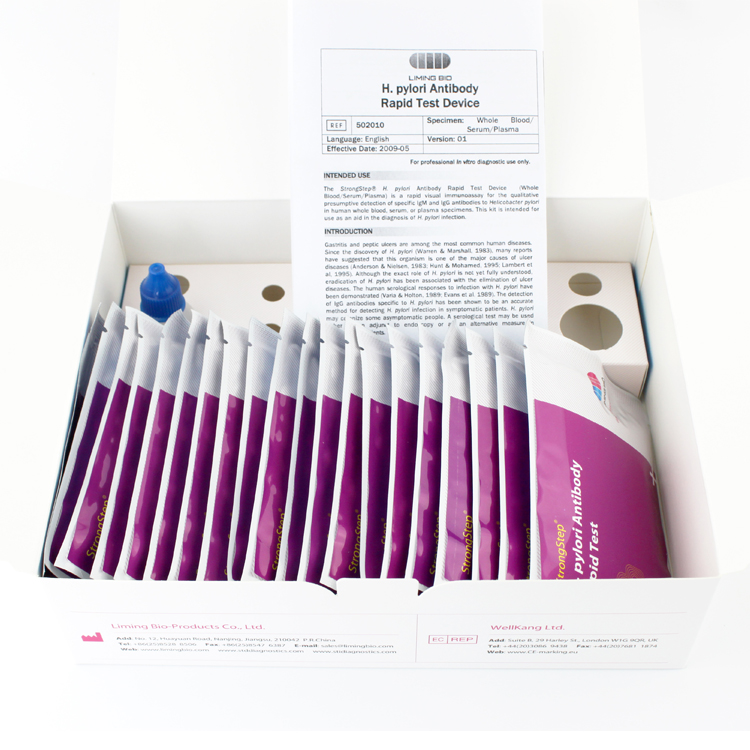
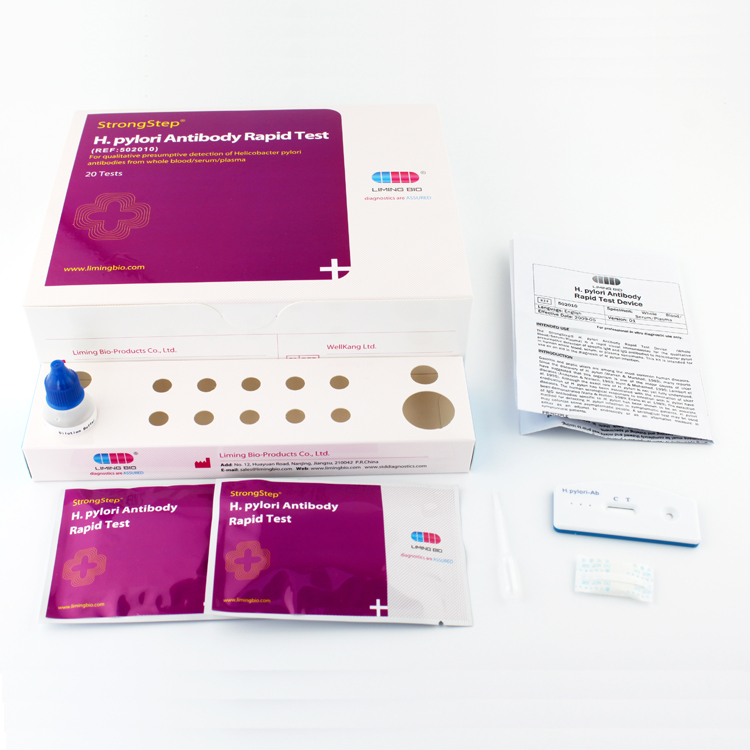
StrongStep® H. pylori Antibody Rapid Test is a rapid visual immunoassay for the qualitative presumptive detection of specific IgM and IgG antibodies to Helicobacter pylori with human whole blood/serum/plasma as specimen.
Benefits
Rapid and convenient
Fingertip blood can be used.
Room temperature
Specifications
Sensitivity 93.2%
Specificity 97.2%
Accuracy 95.5%
CE marked
Kit Size=20 tests
File: Manuals/MSDS
INTRODUCTION
Gastritis and peptic ulcers are among the most common human diseases. Since the discovery of H. pylori (Warren & Marshall, 1983), many reports have suggested that this organism is one of the major causes of ulcer diseases (Anderson & Nielsen, 1983; Hunt & Mohamed, 1995; Lambert et al, 1995). Although the exact role of H. pylori is not yet fully understood, eradication of H. pylori has been associated with the elimination of ulcer diseases. The human serological responses to infection with H. pylori have been demonstrated (Varia & Holton, 1989; Evans et al, 1989). The detection of IgG antibodies specific to H. pylori has been shown to be an accurate method for detecting H. pylori infection in symptomatic patients. H. pylori
may colonize some asymptomatic people. A serological test may be used either as an adjunct to endoscopy or as an alternative measure in symptomatic patients.
PRINCIPLE
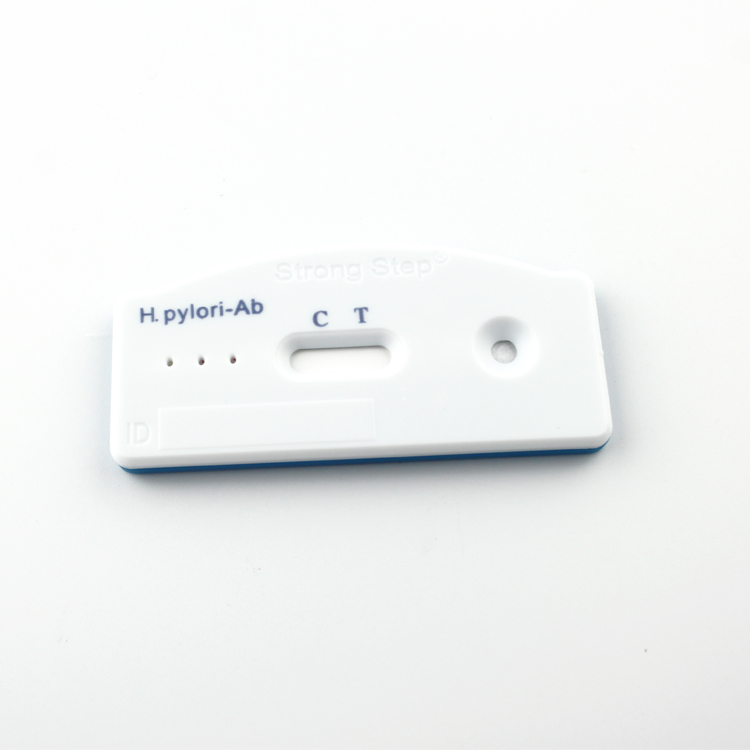
The H. pylori Antibody Rapid Test Device (Whole Blood/Serum/Plasma) detects IgM and IgG antibodies specific to Helicobacter pylori through visual interpretation of color development on the internal strip. H. pylori antigens are immobilized on the test region of the membrane. During testing, the specimen reacts with H. pylori antigen conjugated to colored particles and precoated onto the sample pad of the test. The mixture then migrates through the membrane by capillary action, and interacts with reagents on the membrane. If there are sufficient antibodies to Helicobacter pylori in the specimen, a colored band will form at the test region of the membrane. The presence of this colored band indicates a positive result, while its absence indicates a negative result. The appearance of a colored band at the control region serves as a procedural control, indicating that the proper volume of specimen has been added and membrane wicking has occurred.
PRECAUTIONS
• For professional in vitro diagnostic use only.
• Do not use after the expiration date indicated on the package. Do not use the test if the foil pouch is damaged. Do not reuse tests.
• This kit contains products of animal origin. Certified knowledge of the origin and/or sanitary state of the animals does not completely guarantee the absence of transmissible pathogenic agents. It is therefore, recommended that these products be treated as potentially infectious, and handled by observing usual safety precautions (e.g., do not ingest or inhale).
• Avoid cross-contamination of specimens by using a new specimen collection container for each specimen obtained.
• Read the entire procedure carefully prior to testing.
• Do not eat, drink or smoke in any area where specimens and kits are handled. Handle all specimens as if they contain infectious agents. Observe established precautions against microbiological hazards throughout the procedure and follow standard procedures for proper disposal of specimens. Wear protective clothing such as laboratory coats, disposable gloves and eye protection when specimens are assayed.
• The specimen dilution buffer contains sodium azide, which may react with lead or copper plumbing to form potentially explosive metal azides. When disposing of specimen dilution buffer or extracted samples, always flush with copious quantities of water to prevent azide buildup.
• Do not interchange or mix reagents from different lots.
• Humidity and temperature can adversely affect results.
• Used testing materials should be discarded according to local regulations.
LITERATURE REFERENCES
1. Andersen LP, Nielsen H. Peptic ulcer: an infectious disease? Ann Med. 1993 Dec; 25(6): 563-8.
2. Evans DJ Jr, Evans DG, Graham DY, Klein PD. A sensitive and specific serologic test for detection of Campylobacter pylori infection. Gastroenterology. 1989 Apr; 96(4): 1004-8.
3. Hunt RH, Mohamed AH. The current role of Helicobacter pylori eradication in clinical practice. Scand J Gastroenterol Suppl. 1995; 208: 47-52.
4. Lambert JR, Lin SK, Aranda-Michel J. Helicobacter pylori. Scand J Gastroenterol Suppl. 1995; 208: 33-46.
5. ytgat GN, Rauws EA. The role of Campylobacter pylori in gastroduodenal diseases. A "believer"'s point of view. Gastroenterol Clin Biol. 1989;13(1 Pt 1): 118B-121B.
6. Vaira D, Holton J. Serum immunoglobulin G antibody levels for Campylobacter pylori diagnosis. Gastroenterology. 1989 Oct; 97(4):1069-70.
7. Warren JR, Marshall B. Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet. 1983; 1: 1273-1275.
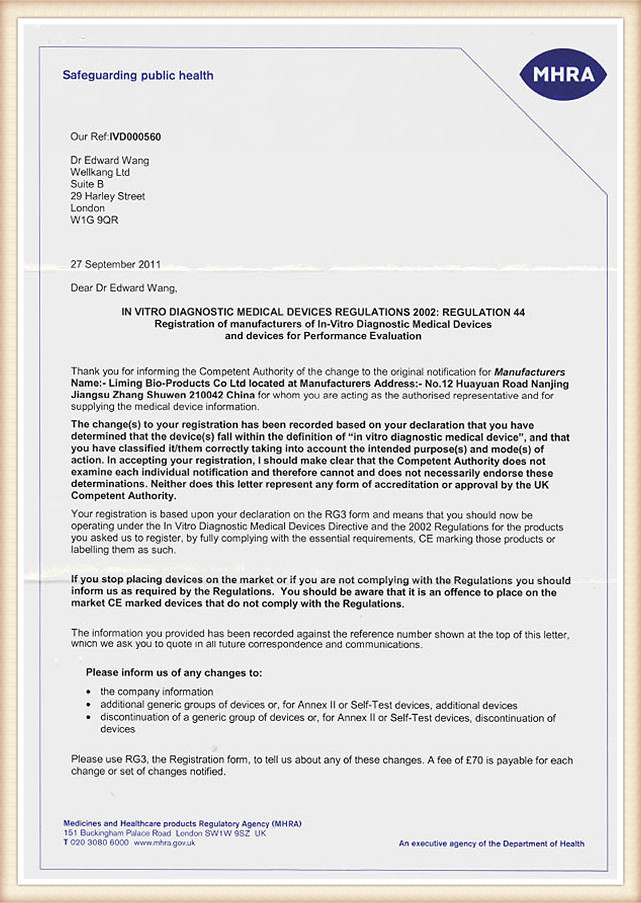
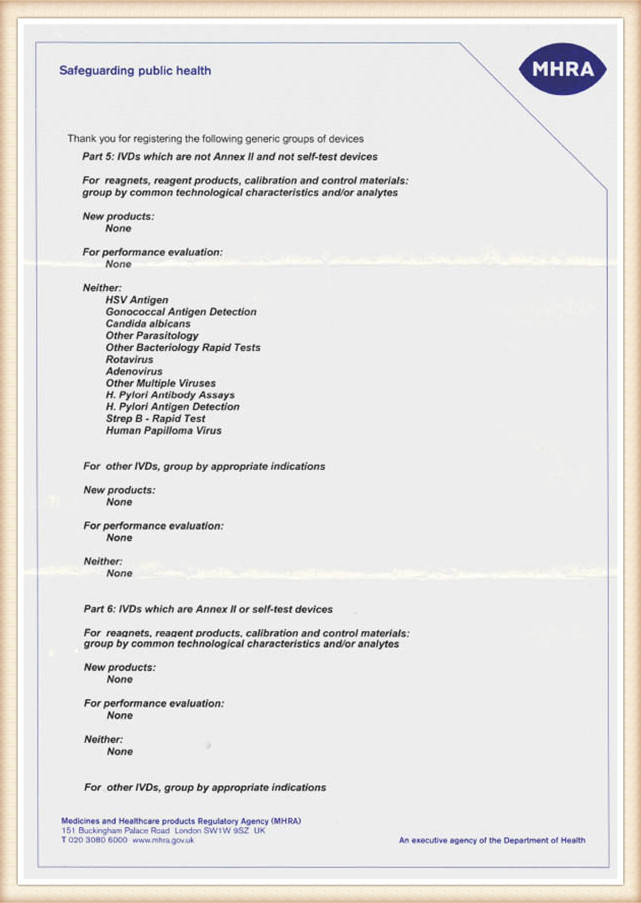
Certifications